Have you ever wondered why your skin reacts differently than others to cuts or bugs or even skincare products? It’s not random. Trust me; there’s a method to that invisible madness—it’s all about your skin’s immunity. You’ve probably heard about the body’s immune system as the noble knight defending you against germs and sickness. Well, your skin’s got its own little army doing a similar job. So, let’s unpack the mystery of skin immunity—it’s like a science story that pertains directly to how we live.
The Invisible Shield: Skin Immunity Decoded
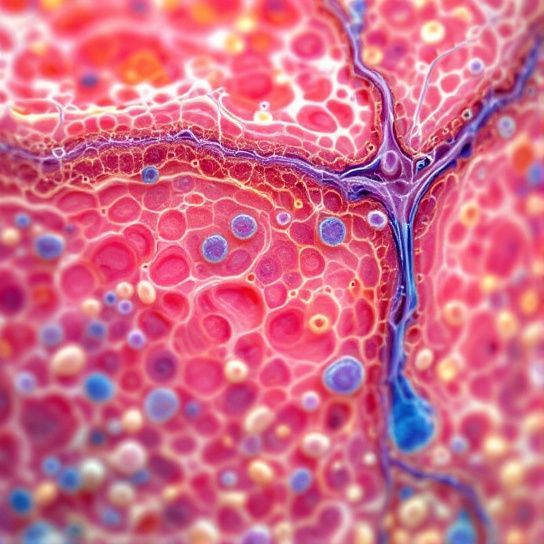
When you think of immunity, your first thought might be white blood cells waging epic battles against viruses and bacteria. But hey, don’t forget your skin—it’s the frontline of defense! Essentially, skin immunity is your body’s way of protecting your insides from outside threats, be they microscopic invaders or environmental sparks. This job requires a squad: cells, proteins, and your skin barrier all working together like synchronized swimmers, striving to keep your defenses robust.
So, why should you care? Well, understanding how this works could help you better manage skin conditions, allergic reactions, and even improve how you treat your skin day to day. Let’s dig deeper into the types that make up this defense system.
Breaking It Down: Innate vs. Adaptive Immunity
Now, onto the nitty-gritty—skin immunity consists of two main parts: innate and adaptive immunity. Imagine innate immunity as your skin’s first responders—like those quick-thinking friends who always know what to do in an emergency. It acts fast, recognizing patterns and providing immediate defense without needing prior experience with the invader.
Next, meet adaptive immunity, the seasoned veterans in your immune system family. They’re like that wise uncle who’s seen everything and reacts based on experience. This type modulates its response based on memory, so if a bacteria or virus attempts a sneak attack, adaptive immunity remembers them vividly and is ready to neutralize them faster.
Innate Immunity: The Immediate Protector
Innate immunity includes physical barriers like the skin surface itself, which blocks toxins and pathogens right off the bat. Then you’ve got cells like Langerhans cells curiously scanning for intruders, and proteins providing immediate retaliation, undermining any attacker’s efforts at causing havoc. Efficient? Indeed.
But don’t get too comfortable—you can’t rely on innate immunity alone to fight prolonged battles. Sometimes these initial barriers get breached, weaving bouts of inflammation or itching, triggering the adaptive responders.
Adaptive Immunity: The Strategic Arsenal
Adaptive immunity is fascinating, marked by its specificity. It’s personalized warfare, targeting pathogens with precision. The secret sauce here? The lymphocytes, also known as B and T cells. B cells create antibodies that hunt down invaders, while T cells come armed with strategies to sin and eliminate corrupted cells.
The way adaptive immunity adapts is quite remarkable and key in fighting serious infections and certain skin maladies. However, its precise response can sometimes go awry, leading to autoimmune responses where the defense hits friendly targets—cue conditions like psoriasis and lupus.
So, What Triggers These Responses?
Here’s where things get funky: triggers vary greatly. Everybody’s skin story is unique, handled differently based on genetics and environmental factors. Ever noticed why your friend glows blissfully in the sun while you break out after a brief exposure? That’s what we call differential skin immunity—and it hugely influences your allergic and inflammatory responses.
Common Triggers
- Environmental Factors: Sunlight, pollution, and even indoor air quality can spur the skin’s defense mechanisms. UV exposure, for example, induces the production of inflammatory cytokines, making our skin more vulnerable.
- Nutrition and Lifestyle: Your diet, stress level, and sleep patterns have a tangible impact. Intake of vitamins, particularly A, C, and E, boosts barrier repair, whereas chronic stress can suppress immune function.
- Aging: As we age, changes in our skin occur at multiple levels. Anecdotally, older skin tends to have increased susceptibility to infections and slower wound healing due to a dwindled immune capability.
Isn’t skin science seriously riveting? And hang on, there’s more nuances to unravel—common conditions linked to misfiring immunity!
Common Skin Conditions and Immunity

Understanding the connection between skin conditions and skin immunity can be enlightening and oddly satisfying. The “aha!” moments offer practical insights into maintaining healthy skin, treating ailments, and even preventing conditions from recurring.
Allergic Reactions: Rashes, Hives, and You
Ever faced red, itchy skin after touching an alien product or eating particular food? Yeah, relatable. Such reactions mean your immune cells identified a harmless substance as hostile, an overzealous move that led to your hives or dermatitis.
To manage this, consider patch tests with new products or dive into identifying allergens by keeping a skin diary for tracking exposure. You’ll thank yourself later!
Psoriasis: When Your Immunity Overreacts
Psoriasis epitomizes the case of immunity gone wild—red, scaly patches arise due to hyperactive T cells escalating rapid skin cell growth. While incurable, there’s a palette of treatments that manage it well, from topical steroids to systemic immunosuppressants.
Balancing immune stimulation, surprisingly, can also come through lifestyle shifts like reducing stress or adopting an anti-inflammatory diet.
Nourishing Your Skin and Its Defenders
Now that you’re equipped with knowledge on skin immunity, it’s time to bolster those defenses. You already know the cornerstone of good skin—cleansing and moisturizing, but allowing your skin the necessary “tools” is critical.
Eat Skin-Friendly Fare
Among friends or alone, feel free to feast on foods rich in omega-3 fatty acids (like salmon or flaxseeds), antioxidants (think berries or dark chocolate), and maintain hydration. They nurture your skin while fortifying its barrier, paving ways for smoother, softer skin tone.

Revitalize Skincare Sensibly
Ever thought less is more? Yep. Overdoing skincare products can irritate/sensitize skin unnecessarily.
- Gentle Cleanser: Aim for cleansers free from harsh sulfates.
- Targeted Serums: Incorporate products with niacinamide or ceramides—they work wonders for barrier repair.
- Protected SPF: No skipping sunscreen. Just don’t!
A Dash of Rest and Relax
Prioritize sleep and carve niches for relaxation. Good sleep literally rebuilds your immunity, providing day-to-day protection from stress elastically impacting emotional and literal skin wellness.
To Wrap It Up Nicely…
In understanding skin immunity types, you’re not just mastering science, my friend, you’re equipping yourself for a healthier and happier skin journey. Each skin type calls for compassion and a bit of experimentation—navigating triggers, drawing insight from them, hopefully transforming knowledge into healthier habits.
And remember, no perfect script here, just give yourself grace. Utilize this understanding as a tool, wading through transformative potential. It feels pretty good being partnered with your skin, knowing you’re its secret ally, whispering defense strategies in your best Adventure Team dreams.
Cherish that skin! It shall cherish you benevolently back.
Frequently Asked Questions
What is skin immunity?
Skin immunity refers to the skin’s ability to resist infections from pathogens. It involves both a passive physical barrier and active components of the innate and adaptive immune systems. The skin contains various immune-competent cells, such as Langerhans cells, keratinocytes, and dendritic cells, which work together to protect against environmental toxins, microbes, and other stresses[1][3][5>.
How does the skin act as an immune organ?
The skin acts as an immune organ through a network of immune-competent cells and soluble biologic response modifiers, including cytokines. Langerhans cells in the epidermis capture, process, and present antigens to T lymphocytes, while keratinocytes produce cytokines like TNFα and IL-1 to enhance immune responses. The dermis contains lymphocytes, macrophages, and other migrant leukocytes that contribute to the immune defense[1][3][5>.
What role does skin microbiota play in skin immunity?
Skin microbiota plays a crucial role in tissue homeostasis and local immunity. The skin’s microbial communities help modulate the host’s immune response and are essential for protecting against infections. For example, the presence of commensals like *Staphylococcus epidermidis* enhances IL-1 signaling and amplifies local inflammatory responses, which is vital for maintaining skin immunity[1][5>.
How is skin immunity affected by disruptions in the skin barrier?
Disruptions in the skin barrier, such as those seen in conditions like eczema, psoriasis, and rosacea, can significantly impair skin immunity. The integrity of the stratum corneum and the presence of lipids and antimicrobial peptides are critical for maintaining the skin’s barrier function. When this barrier is compromised, the skin becomes more vulnerable to infections and inflammatory responses[1][4][5>.
References


